The Overlap Between FND, ME/CFS, and Fibromyalgia: The Challenge of Clear Diagnosis
- FND Health

- Oct 4, 2024
- 5 min read
Updated: Jan 23
If you've ever experienced symptoms like chronic fatigue, pain, or neurological disturbances and sought help from different specialists, you might have encountered a frustrating reality: one doctor might diagnose you with Functional Neurological Disorder (FND), another with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), and yet another with fibromyalgia. How can the same symptoms lead to different diagnoses? And what does that say about these conditions?
It highlights something crucial—these disorders share many common features, and their root cause may lie in nervous system dysregulation.
The Similarities: More Than Just Fatigue and Pain
All three conditions—FND, ME/CFS, and fibromyalgia—are complex, multi-system disorders that affect day-to-day functioning in profound ways. Here's what they often have in common:
Chronic fatigue: A hallmark of both ME/CFS and fibromyalgia, this overwhelming fatigue doesn't resolve with rest. FND patients also report significant fatigue, though it often comes alongside neurological symptoms.
Pain: Fibromyalgia is defined by widespread pain, but patients with ME/CFS and FND can also experience pain as a symptom. In all cases, the pain seems to stem from nervous system dysfunction rather than any identifiable damage to tissues.
Cognitive symptoms: Brain fog, trouble concentrating, and memory issues are common in all three conditions, whether it's called "fibro fog" in fibromyalgia or "post-exertional neuroimmune exhaustion" in ME/CFS.
Sleep disturbances: Patients across all these conditions often struggle with unrefreshing sleep, which only adds to their fatigue. Many also report experiencing vivid nightmares, further disrupting their ability to get restorative rest.
Sensitivity to stress: Whether it's emotional stress, physical exertion, or illness, the nervous systems of people with these conditions seem to overreact, triggering a cascade of symptoms.
Different Specialists, Different Diagnoses
The difficulty in getting a clear diagnosis often lies in the fact that each specialist views these symptoms through a different lens:
A neurologist might focus on the neurological symptoms—weakness, tremors, seizures, or movement difficulties—and diagnose FND, which is characterized by abnormal nervous system functioning, even though no structural abnormalities are found in the brain or spine.
A doctor experienced in ME/CFS might zero in on the debilitating fatigue, post-exertional malaise (where symptoms worsen after minimal effort), and immune dysfunction. The diagnosis of ME/CFS tends to focus on these energy deficits, but there’s a growing recognition that nervous system dysfunction plays a role here too.
If widespread pain is the primary concern, a rheumatologist or pain specialist may diagnose fibromyalgia. This condition is often diagnosed based on widespread pain and tenderness in specific areas, along with fatigue and sleep issues.
The overlap in symptoms can make it difficult for doctors to agree on a single diagnosis, leaving patients feeling confused and frustrated. In many cases, patients end up receiving multiple diagnoses over time, as they bounce between specialists.

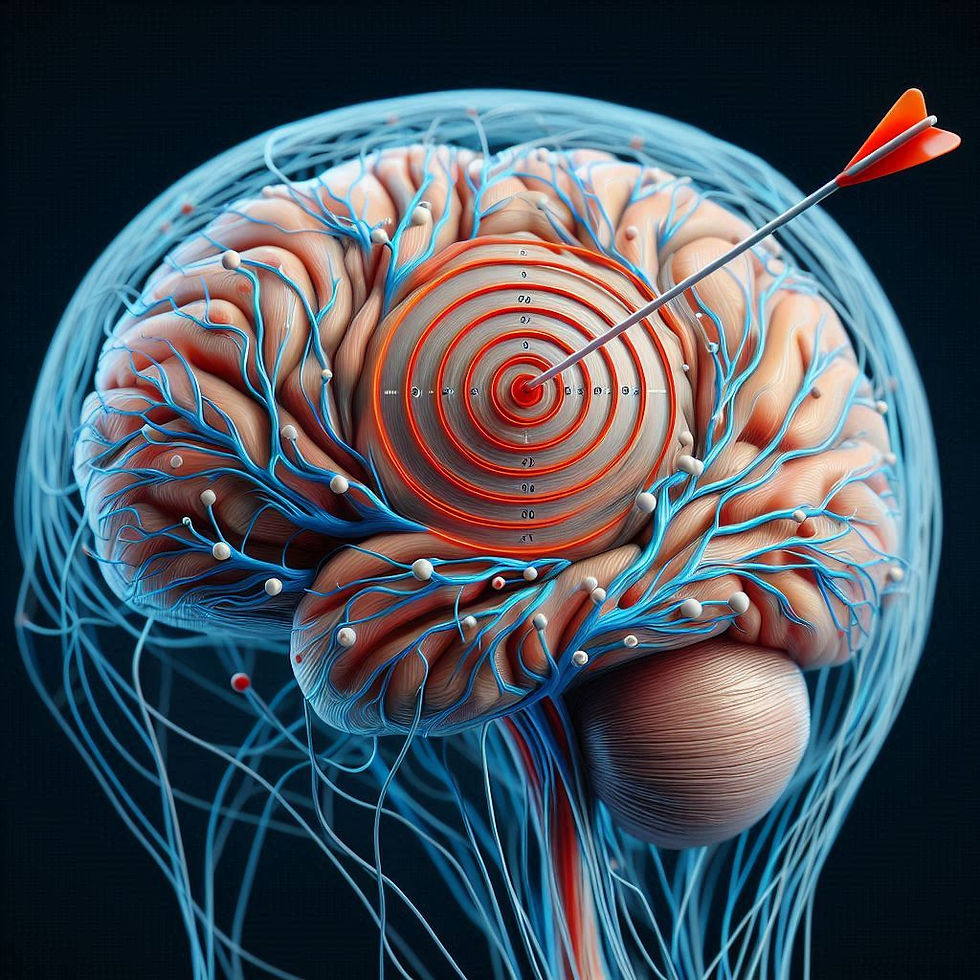
A Common Root: Nervous System Dysregulation?
Despite the differences in diagnoses, one thing is clear: these conditions likely share a common underlying mechanism—dysregulation of the nervous system.
The nervous system controls much more than just movement and reflexes; it also manages our response to stress, regulates immune function, and balances hormones. When it becomes hypersensitive—whether due to trauma, chronic stress, infections, or other triggers—it can misfire, leading to a range of symptoms like pain, fatigue, and neurological disturbances.
Some research has shown that people with these conditions have overactive sympathetic nervous systems (the fight-or-flight system), alongside a weakened parasympathetic response (the rest-and-digest system) . This imbalance can leave the body in a state of chronic hyperarousal, where even small stressors or exertions cause major symptom flare-ups.
The Challenge for Patients: A Lack of Consensus
For patients, the lack of a clear diagnosis can be frustrating. It can feel like no one has a full picture of what’s going on, especially when symptoms fall into this grey area where they overlap. Often, patients may feel dismissed, or they may be given a diagnosis that doesn’t capture the entirety of their experience.
But this overlap also opens up a new way of thinking about these disorders. Rather than focusing solely on the differences, understanding that they share common features could lead to more effective treatments. Targeting the nervous system—through brain training exercises, calming techniques, pacing, and diet—could help manage symptoms across the board.
Why Do Some People with ME/CFS Consider It a Physical Disease?
Many individuals with ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome) believe their condition is distinctly different from other functional disorders, like FND, even though no disease markers have been consistently identified. Some patients find it difficult to see ME/CFS as a functional disorder because of the severe, life-altering physical symptoms they experience, such as extreme fatigue, immune dysfunction, and post-exertional malaise. However, it’s important to recognize that FND and other conditions like fibromyalgia also involve similarly severe physical and neurological symptoms.
The reality is that ME/CFS, like FND and fibromyalgia, is a functional disorder. All of these conditions involve dysregulation in how the body’s systems—particularly the nervous system—function, rather than identifiable structural damage.
Here’s why:
No Identifiable Structural Damage: Just like in FND, there is no consistent evidence of structural abnormalities in ME/CFS. Standard diagnostic tests, such as imaging and blood tests, typically do not reveal any physical damage to organs or tissues—this is a hallmark of functional disorders.
Nervous System Dysregulation: Both ME/CFS and FND involve underlying dysfunctions in how the nervous system regulates the body. In ME/CFS, this often manifests as problems with energy regulation and immune response, while in FND, the miscommunication between the brain and body leads to physical and neurological symptoms such as weakness, tremors, or seizures. FND involves real, measurable dysfunction in the way the nervous system operates, which results in various physical and neurological symptoms, despite the lack of structural damage. Similarly, ME/CFS involves a breakdown in how the body manages energy and stress, driven by the nervous system.
Shared Functional Features: Like FND, ME/CFS is considered a functional disorder because the root of the issue lies in how the body functions, not in structural damage. Even though the symptoms are physically felt, they are driven by a disruption in how the body’s systems—especially the nervous system—communicate and regulate themselves.
This distinction is important because it shifts the focus away from thinking of ME/CFS as a purely physical disease and aligns it with other functional disorders like FND. Recognizing that ME/CFS, despite its severe symptoms, is a functional disorder helps direct research and treatment toward managing the underlying nervous system dysregulation, rather than searching for structural damage that isn’t there.

Conclusion
The overlap between FND, ME/CFS, and fibromyalgia reminds us how little we still understand about the human body—especially the nervous system. Yet, it also provides a glimmer of hope. By focusing on the common thread of nervous system dysfunction, patients may find a path forward that emphasizes holistic care, slow progress, and gentle retraining of the nervous system.
No matter the diagnosis, the journey to understanding and healing involves recognizing that these symptoms are real, complex, and valid—even if they don’t fit neatly into one diagnostic box.
References:
Institute of Medicine (US) Committee on the Diagnostic Criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness. Washington (DC): National Academies Press (US); 2015.
Stone, J., Carson, A., & Sharpe, M. (2009). Functional symptoms and signs in neurology: assessment and diagnosis. Journal of Neurology, Neurosurgery & Psychiatry, 80(12), 1276-1283. doi:10.1136/jnnp.2008.171306
Clauw, D. J. (2014). Fibromyalgia: A clinical review. JAMA, 311(15), 1547–1555. doi:10.1001/jama.2014.3266
American Academy of Sleep Medicine. (2014). International Classification of Sleep Disorders (3rd ed.). Darien, IL: American Academy of Sleep Medicine.
Van Heugten-van der Kloet, D., Giesbrecht, T., & Merckelbach, H. (2015). Nightmare frequency is associated with subjective sleep quality but not with psychopathology. Sleep Medicine, 16(3), 340-342. doi:10.1016/j.sleep.2014.11.007
---








Comments