How Physical Stress Can Lead to Neurological Disorders: Understanding the Connection
- FND Health

- Jul 1, 2024
- 3 min read
Updated: Jan 20
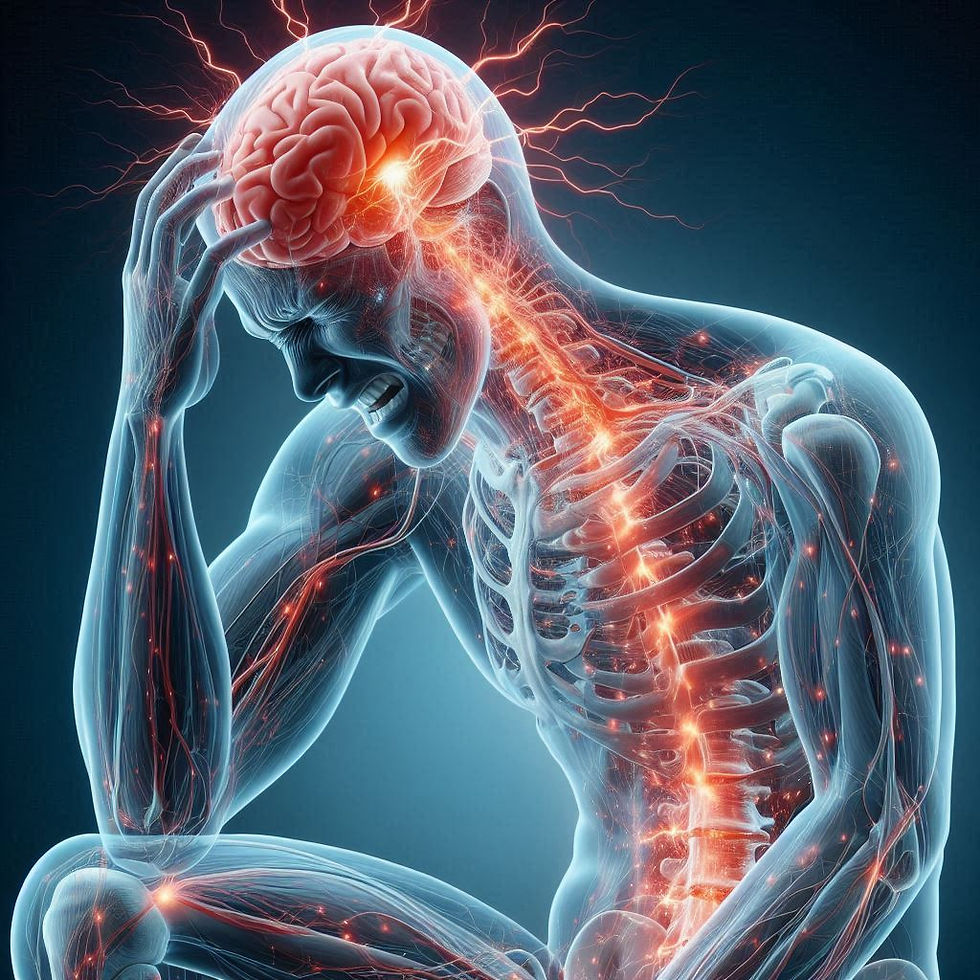
Physical stress, whether from pain, injury, or a virus, can lead to complex interactions between the body and brain, contributing to the development of disorders like fibromyalgia, functional neurological disorder (FND), and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). This blog post explores how these processes might occur.

Mechanisms of Physical Stress Leading to Neurological Conditions
Central Sensitization: Pain and Injury: Persistent pain or injury can lead to central sensitization, where the nervous system becomes hypersensitive. This heightened sensitivity can cause pain to be perceived even in the absence of harmful stimuli, contributing to conditions like fibromyalgia. Chronic Pain Syndromes: The constant barrage of pain signals can alter the functioning of pain pathways in the brain, making it easier for pain signals to be amplified.
Neuroinflammation: Viral Infections: Viruses can trigger an immune response, leading to neuroinflammation. This inflammation can disrupt normal brain function, potentially leading to cognitive and neurological symptoms seen in conditions like ME/CFS.
Cytokine Release: The body’s response to infection or injury often involves the release of cytokines, which can cross the blood-brain barrier and influence brain function, possibly leading to fatigue, pain, and cognitive dysfunction.
Hypothalamic-Pituitary-Adrenal (HPA) Axis Dysregulation: Stress Response: Physical stress can disrupt the HPA axis, leading to imbalances in cortisol and other stress hormones. These imbalances can affect the brain's ability to regulate mood, pain, and energy levels, contributing to conditions like fibromyalgia and ME/CFS. Chronic Stress: Prolonged activation of the stress response system can lead to a state of chronic stress, which is associated with both physical and psychological symptoms.
Autonomic Nervous System (ANS) Dysfunction: Dysregulation: Physical stressors can lead to dysfunction of the autonomic nervous system, affecting heart rate, blood pressure, and other vital functions. This can contribute to symptoms like dizziness, fatigue, and cognitive impairment often seen in FND and ME/CFS.
Postural Orthostatic Tachycardia Syndrome (POTS): Some patients with ME/CFS exhibit POTS, where the ANS fails to properly regulate blood flow and blood pressure, leading to various neurological symptoms.
Mitochondrial Dysfunction: Energy Production: Physical stress, especially from viral infections, can impair mitochondrial function, reducing the body's ability to produce energy efficiently. This can lead to the profound fatigue and muscle pain characteristic of ME/CFS and fibromyalgia.
Oxidative Stress: Mitochondrial dysfunction can also increase oxidative stress, damaging cells and tissues, including those in the brain, contributing to neurological symptoms.
Neuroplasticity and Maladaptive Learning:
Brain Changes: Chronic pain and stress can lead to changes in brain structure and function through processes of neuroplasticity. These changes can make the brain more prone to perceiving pain and other symptoms even in the absence of an obvious physical cause.
Maladaptive Networks: The brain may develop maladaptive neural networks that perpetuate symptoms, as seen in FND, where patients experience neurological symptoms without an identifiable organic cause.
Example: From Whiplash to Fibromyalgia or FND
Consider a scenario where an individual suffers whiplash from a car accident. Here’s how this injury could potentially lead to fibromyalgia or FND:
Initial Injury: The whiplash causes significant pain and physical stress, leading to acute inflammation and tissue damage.
Persistent Pain: As the initial injury heals, the individual continues to experience persistent neck pain. This ongoing pain can lead to central sensitization, where the nervous system becomes increasingly sensitive to pain.
Chronic Stress: The continued pain and stress from dealing with the injury can disrupt the HPA axis, leading to imbalances in stress hormones like cortisol. This disruption can contribute to widespread pain and fatigue, key symptoms of fibromyalgia.
Autonomic Dysfunction: The physical trauma and ongoing stress can also affect the autonomic nervous system, leading to symptoms like dizziness, fatigue, and cognitive impairment, which are often seen in FND.
Neuroplastic Changes: Over time, the brain may adapt to the persistent pain and stress by developing maladaptive neural networks. These changes can make the brain more prone to perceiving pain and other neurological symptoms, even in the absence of ongoing physical injury.
Conclusion
The development of disorders like fibromyalgia, FND, and ME/CFS often involves a complex interplay of physical and neurological factors. While they can start with a physical stressor, such as an injury, the subsequent changes in brain function can perpetuate and amplify symptoms, leading to the chronic and often debilitating nature of these conditions. Understanding these mechanisms can help in developing better treatment strategies that address both the physical and neurological aspects of these disorders.
References
Clauw, D. J. (2014). Fibromyalgia: A clinical review. JAMA, 311(15), 1547-1555. DOI:10.1001/jama.2014.3266
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W., & Kelley, K. W. (2008). From inflammation to sickness and depression: When the immune system subjugates the brain. Nature Reviews Neuroscience, 9(1), 46-56. DOI:10.1038/nrn2297
VanElzakker, M. B., Brumfield, S. A., & Lara Mejia, P. S. (2019). Neuroinflammation and Cytokines in ME/CFS. Frontiers in Neurology, 10, 1022. DOI:10.3389/fneur.2019.01022
Reynolds, G. K., Lewis, D. P., & Richardson, A. M. (2014). A systematic review of the psychological treatment of functional neurological disorders. Journal of Psychosomatic Research, 77(1), 1-12. DOI:10.1016/j.jpsychores.2014.04.013







Comments